Lipitor (atorvastatin) is a prescription medicine that lowers cholesterol in the blood. It belongs to a class of medications called HMG-CoA reductase inhibitors, also called statins. Lipitor helps decrease the fatty substances such as LDL-C (“bad” cholesterol) and triglycerides in the blood and helps increase the amount of HDL-C (“good” cholesterol). Lipitor is for adults and children 10 years and older whose cholesterol levels are high despite of exercise and a low-fat diet.
Lipitor helps lower the risk for heart attack, stroke, certain types of heart surgery, and chest pain in patients who have heart disease or risk factors for heart disease such as old age, smoking, high blood pressure, low HDL-C, and hereditary heart disease. It can also lower the risk for heart attack or stroke in patients diagnosed with diabetes and risk factors such as eye problems, kidney problems, smoking, or high blood pressure.
Prescription Name and Overview
Lipitor is taken orally with or without food, depending on the doctor’s advice. Usually, this drug is taken once a day.
The recommended dose is 10-80 mg daily. The dosage of this medication depends on a person’s age, medical condition, rate of response to the medication, and other medications being taken. It is advised to take this medication at the same time every day in order to get the most benefit from it.
Lipitor should be used together with proper diet, exercise, and weight loss to lower the risk of heart attack, stroke, and the chance of needing heart surgery. Proper diet is necessary to lower bad cholesterol and fats (LDL, triglycerides), and increase good cholesterol (HDL). It may take up to 2 weeks before a person feels the full benefit of the drug.
Generic Name and Overview
Atorvastatin, the generic name of Lipitor, is available in the market. On November 30, 2011, Watson Pharmaceuticals and Ranbaxy Pharmaceuticals were approved by the FDA to produce atorvastatin at much more affordable prices. But it was not until 2012, when other manufacturers began to supply the generic drug that the price of the medication dropped.
John Santa, MD, MPH, director of the Consumer Reports Health Ratings Center states that the generic version of Lipitor is the same as the brand-name counterpart. “The FDA imposes strict manufacturing parameters on the makers of generic drugs,” Santa says. He adds that, “And when you look back at the manufacturing problems that have occured, they are just as likely at a brand-name plant as at a generic plant.”
OTC Name and Overview
Both Lipitor and its generic counterparts are not available as over-the-counter medications; they are available only through a doctor’s prescription.
Manufacturer
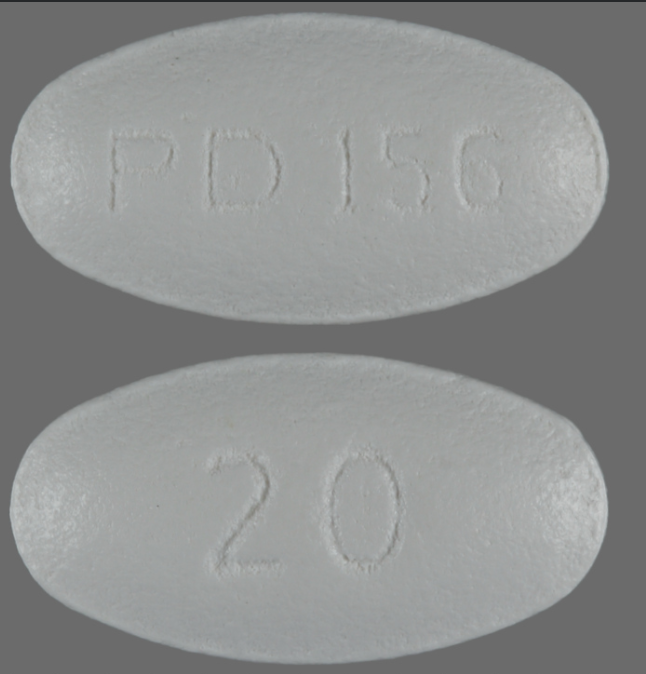
Pfizer is the manufacturer of Lipitor.
Labeled Indications
Lipitor is an inhibitor of HMG-CoA reductase (statin) indicated as an adjunct therapy to diet.
- Prevention of Cardiovascular Disease in Adults
Adult patients who have no clinically evident coronary heart disease (CHD), but have multiple risk factors for CHD due to age, smoking, hypertension, low HDL-C, or a family history of coronary heart disease, Lipitor is indicated to:
- Lower the risk of MI (myocardial infarction)
- Lower the risk of stroke
- Lower the risk of revascularization procedures and angina
Adult patients who are diagnosed with type 2 diabetes and who have no evident coronary heart disease, but have multiple risk factors for coronary heart disease such as retinopathy, albuminuria, smoking, or hypertension, Lipitor is indicated to:
- Lower the risk of myocardial infarction
- Lower the risk of stroke
Adult patients who are diagnosed with coronary heart disease, Lipitor is indicated to:
- Lower the risk of non-fatal myocardial infarction
- Lower the risk of fatal and non-fatal stroke
- Lower the risk of revascularization procedures
- Lower the risk of hospitalization for CHF
- Lower the risk of angina
LIpitor is indicated:
- As an adjunct diet to reduce elevated total-C, LDLC-C, apo B, and TG levels and to increase HDL-C in patients with primary hypercholesterolemia and mixed dyslipidemia (Fredrickson Types IIa and IIb);
- As an adjunct to diet for the treatment of patients with elevated serum TG levels (Fredrickson Type IV);
- For the treatment of patients with primary dysbetalipoproteinemia (Fredrickson Type III) who do not respond adequately to diet;
- To reduce total-C and LDL-C in patients with homozygous familial hypercholesterolemia as an adjunct to other lipid-lowering treatments (e.g., LDL apheresis) or if such treatments are unavailable;
- As an adjunct to diet to reduce total-C, LDL-C, and apo B levels in boys and postmenarchal girls, 10 to 17 years of age, with heterozygous familial hypercholesterolemia if after an adequate trial of diet therapy the following findings are present:
- LDL-C remains ≥190 mg/dL or
- LDL-C remains ≥160 mg/dL and:
- There is a positive family history of premature cardiovascular disease or
- Two or more other CVD risk factors are present in the pediatric patient
Active Ingredients
Atorvastatin calcium is the active ingredient found in Lipitor.
What Is It Used For?
The official website of Lipitor states that “Lipitor is a prescription medicine that lowers cholesterol in the blood. It lowers the LDL-C (“bad” cholesterol) and triglycerides in your blood. It can raise your HDL-C (“good” cholesterol) as well. Lipitor is for adults and children over 10 whose cholesterol does not come down enough with exercise and a low-fat diet alone.”
The website also states that “Lipitor can lower the risk for heart attack, stroke, certain types of heart surgery, and chest pain in patients who have heart disease or risk factors for heart disease such as age, smoking, high blood pressure, low HDL-C, or heart disease in the family. Lipitor can lower the risk for heart attack or stroke in patients with diabetes and risk factors such as eye problems, kidney problems, smoking, or high blood pressure.”
How Does it Work?
Lipitor is a statin. It works by slowing down the production of cholesterol in the body to decrease the amount of cholesterol that may build up on the walls of the arteries and block blood flow to the heart, brain, and other parts of the body.
When cholesterol and fats accumulate along the walls of the arteries, blood flow is decreased. The amount of oxygen reaching the heart, brain, and other parts of the body are decreased and may cause heart disease, angina (chest pain), strokes, and heart attacks.
What are the Approved Uses?
Lipitor is approved for use as an adjunct therapy to diet to:
- Reduce the risk of myocardial infarction (MI), stroke, revascularization procedures, and angina in patients without CHD, but with multiple risk factors
- Reduce the risk of MI and stroke in patients with type 2 diabetes without CHD, but with multiple risk factors
- Reduce the risk of non-fatal MI, fatal and non-fatal stroke, revascularization procedures, hospitalization for CHF, and angina in patients with CHD
- Reduce elevated total-C, LDL-C, apo B, and TG levels and increase HDL-C in adult patients with primary hyperlipidemia and mixed dyslipidemia
- Reduce elevated TG in patients with hypertriglyceridemia and primary dysbetalipoproteinemia
- Reduce total-C and LDL-C in patients with homozygous familial hypercholesterolemia
- Reduce elevated total-C, LDL-C and apo B levels in boys and postmenarchal girls, 10 to 17 years of age, with heterozygous familial hypercholesterolemia after failing in adequate trial of diet therapy.
Production Anecdotes / History
In 1986, atorvastatin was first patented. In 1996, Pfizer was first approved to manufacture Lipitor for medical use in the United States.
Statins are the most popularly prescribed medication in the United States, and Lipitor is the top-selling prescription medication of all time, exceeding $130 B in sales. As of today, there are more than 29 million people in the US alone who have been given a Lipitor prescription.
Precautions
Some precautions to follow:
- Before taking Lipitor, inform your doctor if you are allergic to any of the ingredients in the Lipitor tablet.
- Before taking Lipitor, tell your doctor of any other medications you are taking, or any vitamin supplement, over-the-counter drug, herbal products you are taking or are planning to take.
- Tell your doctor if you have liver disease. You will go through a series of laboratory tests so that the doctor will see if your liver is working well even if you do not think you have liver disease. Your doctor will not let you take this drug if you have liver disease, have had liver disease, or if the tests show you have a developing liver disease.
- Inform you doctor if you are 65 years of age or older, if you consume more than 2 alcoholic beverages in a day, if you have had muscle aches or weakness, diabetes, seizures, low blood pressure, thyroid disease, or kidney disease.
- Inform your doctor if you are pregnant or are planning to become pregnant. If you become pregnant while under this medication, stop taking Lipitor and call your doctor of your situation immediately. This drug may cause harm to the unborn baby.
- It is not established if this medication passes through breast milk. Because of possible risks to the baby, do not breastfeed while taking this drug.
- Should you be hospitalized for any injury, infection, surgery (including dental surgery), and other medical emergencies, inform the medical professional who is treating you that you are taking this drug.
- Alcohol can increase the risks associated with the side effects of this drug. Ask your doctor about the safe amount of alcohol you are allowed to take, or stop consuming alcohol altogether.
- Lipitor, like other statins, occasionally causes myopathy, defined as muscle aches or muscle weakness in conjunction with increases in creatinine phosphokinase (CPK) values >10 times ULN. the concomitant use of higher doses of atorvastatin with certain drugs such as cyclosporine and strong CYP3A4 inhibitors increase the risk of myopathy/rhabdomyolysis.
Long-Term Use Considerations
Clinical studies have shown that although there are numerous benefits from Lipitor, the side effects of drug become more apparent only after long-term use. Some of these considerations are:
- Liver Problems- in a small percentage of patients, Lipitor elevates the liver enzymes within the first few months of starting the drug. The elevation of the liver enzymes are reversible upon the discontinuation of the drug. This is the reason why doctors prescribe a lower dose for most patients at the start.
Because of this elevation of liver enzymes within the first few months of taking the drug, concerns have been raised about the potential long-term effects of Lipitor on the liver. There are reports of some reports of liver failure happening in a few patients. Although there is no established link between Lipitor and liver failure, the drug should not be used in patients with liver disease.
- Muscle Problems-a common side-effect of statin drugs, where Lipitor belongs, is mild muscle pain or myopathy. This is more apparent in people taking cyclosporine or fibric acid derivatives together with Lipitor.
This muscle pains that develop over time from long-term use of Lipitor could signal a disease called rhabdomyolysis. This disease could lead to renal failure and even death. It is important to check the creatinine phosphokinase (CPK) enzyme levels in a patient’s blood regularly.
- Memory Loss- when Lipitor was tested in thousands of patients prior to its approval and commercialization, memory loss was not among the side effects that were detected. However, after millions of patients who have used it over the years, there were some instances where patients complained of experiencing memory loss. Although there is no direct link between Lipitor and memory loss, the rare side effect may be due to long-term use.
Drug Interactions
Drug interactions happen when a substance that you are taking changes or disrupts a drug’s intended function. Interactions may be harmful to you, increase your risk for serious side effects, or inhibit a drug from functioning properly. Always consult a doctor if you are going to start a medication with a new drug.
Can Interact with the Following
The following drugs commonly interacts with Lipitor:
- Aleve (naproxen)
- Amlodipine (Norasc)
- Amoxicillin
- Aspir 81 (aspirin)
- Clarithromycin (Biaxin, Biaxin XL)
- Ubiquinone
- Cymbalta (duloxetine)
- Doxycycline
- Eliquis (apixaban)
- Erythromycin
- Fenofibrate
- Fish oil (omega-3 polyunsaturated fatty acids)
- Gemfibrozil
- Grapefruit
- Ibuprofen
- Januvia
- Lantus
- Levothyroxine
- Lisinopril
- Metoprolol, Metoprolol Succinate ER, Metoprolol Tartrate
- Metronidazole
- Nexium (esomeprazole)
- Niacin
- Plavix (clopidogrel)
- proAir HFA (albuterol)
- Simvastatin
- Synthroid (levothyroxine)
- Tylenol (acetaminophen)
- Viagra (sildenafil)
- Vitamin B12
- Vitamin C
- Vitamin D3
- Wine
- Xarelto (rivaroxaban)
Lipitor also interacts with alcohol.
Can’t Interact with the Following
People who have liver disease, rhabdomyolysis, cognitive impairment, diabetes, and renal disease should take extra precaution, or not take Lipitor at all. Lipitor may worsen the condition of those mentioned above.
Don’t use Lipitor together with:
- Posaconazole
- Ritonavir
There are many drugs that should not be used together with Lipitor. This may include over-the-counter medications, vitamins, supplements, and herbal products. Always ask your doctor if you wish to start or stop using any medication while you are taking this drug.
When To Stop Taking
Do not take Lipitor if you:
- Are pregnant, feel you may be pregnant, or are hoping to become pregnant. If you get pregnant, stop taking this drug immediately and inform your doctor about it. Lipitor may harm the fetus.
- Are breastfeeding. The active ingredients in Lipitor can pass into your breastmilk.
- Have liver disease.
- Are allergic to atorvastatin or any of the ingredients found in Lipitor.
Long-Term Side Effects
Some long-term side effects that are associated with Lipitor are:
- Liver disease
- Muscle problems (myopathy and rhabdomyolysis)
- Memory loss
- Increased blood sugar
FDA Warnings (History Of)
- November 28, 2012- Ranbaxy Ic. initiated a voluntary recall of 41 affected lots of Atorvastatin tablets as a precautionary measure to the fact that the affected lots may contain very small glass particles resembling a grain of sand.
- February 28, 2012- FDA approved the removal of routine monitoring of liver enzymes from drug labels. Added to the labels are the information about potentially non-serious and reversible cognitive side effects of the drug and reports of increased blood sugar and glycosylated hemoglobin levels.
- December 23, 2010- Pfizer recalled one lot of Lipitor 40 mg tablets distributed in the US as a response to complaints of uncharacteristic odor of the tablets.
- October 10, 2010- Pfizer recalled specific bottles of Lipitor 40 mg tablets due to an uncharacteristic odor.
- September 30, 2008- FDA provides new evidence that statins do not increase the incidence of ALS (amyotrophic lateral sclerosis) or Lou Gehrig’s Disease.
Other Common Side Effects
Listed below are some side effects that are caused by Lipitor. If the symptoms are severe and lasts for a long time, call your doctor right away:
- Diarrhea
- Heartburn
- Gas
- Joint pain
- Forgetfulness or memory loss
- Confusion
- Nasopharyngitis
- Arthralgia
- Pain in extremity
- Urinary tract infection
- Insomnia
- Pharyngolaryngeal pain
- Increased blood sugar or type 2 diabetes
Listed below are some uncommon but serious side effects. Call your doctor right away if you experience any of the following:
- Rhabdomyolysis and myopathy
- Liver enzyme abnormalities
- Allergy
Lawsuits
In 2014, Pfizer faced more than 1000 lawsuits involving more than 4,000 female statin users who alleged that Lipitor caused them to have Type 2 Diabetes.
Representatives of the company denied these allegations, stating that these women may have risk factors that increased their vulnerability to diabetes, such as obesity and high blood pressure. The company referred to what they call an “overwhelming consensus” in the medical community about the benefits of statin in defense of Lipitor.
These lawsuits was made after a 2012 order by the FDA to include in the labelling that Lipitor is linked to high blood sugar and increases the risk for type 2 diabetes. In cases like these, plaintiffs allege that the companies who manufacture the drug were aware of the risk that goes with the medication but withheld this information from the public to protect their sales.