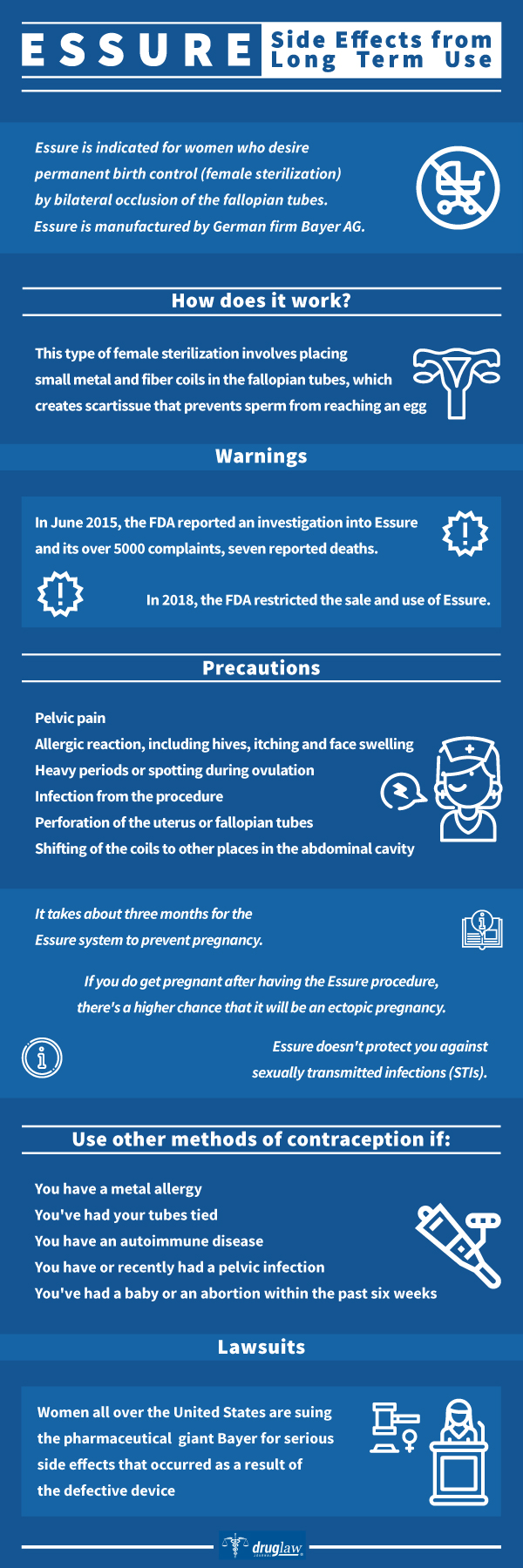
Essure is a form of permanent birth control for women. It is irreversible. This type of female sterilization involves placing small metal and fiber coils in the fallopian tubes, which creates scar tissue that prevents sperm from reaching an egg. During the procedure, the doctor inserts a flexible tube with a small camera (hysteroscope) through the vagina and cervix and up to the uterus. From here, the doctor can see the opening to the fallopian tubes and place the Essure system coils into them.
Prescription Name and Overview
It takes about three months for the Essure system to prevent pregnancy. In some women, it may take up to six months. During this time, you must use another form of birth control to prevent pregnancy. Essure doesn’t protect you against sexually transmitted infections (STIs).
Generic Name and Overview
Both the device and method is commonly known as Essure.
OTC Name and Overview
Manufacturer
Essure is manufactured by German firm Bayer AG.
Labeled Indications
Essure is indicated for women who desire permanent birth control (female sterilization) by bilateral occlusion of the fallopian tubes.
Active Ingredients
The small, flexible inserts are made from polyester fibers, nickel-titanium, stainless steel and solder. The insert contains inner polyethylene terephthalate fibers to induce inflammation, causing a benign fibrotic ingrowth, and is held in place by flexible stainless steel inner coil and a dynamic outer nickel titanium alloy coil. Unlike temporary methods of birth control, the Essure inserts do not contain or release hormones. The inserts do not prevent the transmission of sexually transmitted infections.
What Is It Used For?
Essure is used as a contraceptive.
How Does it Work?
A physician places the coils into the fallopian tubes by a catheter passed from the vagina through the cervix and uterus. Once in place, the ingrowth continues over a period of three months, resulting in durable occlusion or blockage in the Fallopian tubes; the tissue barrier formed is supposed to prevent sperm from reaching an egg. During that intervening three-month period, women are advised to use an alternate contraceptive method.
What are the Approved Uses
The FDA approved Essure as a contraceptive in 2002.
Production Anecdotes / History
Conceptus began marketing Essure in 2002. In June 2013, German firm Bayer AG acquired Conceptus and, in turn, acquired all the rights regarding the marketing and manufacture of Essure.
Precautions
Researchers continue to study the risks associated with or possibly linked to the Essure system. They may include:
- Pelvic pain
- Allergic reaction, including hives, itching and face swelling
- Heavy periods or spotting during ovulation
- Infection from the procedure
- Perforation of the uterus or fallopian tubes
- Shifting of the coils to other places in the abdominal cavity
Sometimes, the coils aren’t placed properly or only one tube becomes blocked. This can result in unintended pregnancy. However, less than 1.5 out of 1,000 women get pregnant with the Essure system. When pregnancy occurs, it’s usually because:
- Pregnancy occurred before the procedure.
- The coils weren’t placed properly.
- Back-up contraception wasn’t used for three to six months following the procedure, or until the doctor confirmed tubal blockage.
If you do get pregnant after having the Essure procedure, there’s a higher chance that it will be an ectopic pregnancy — when fertilization happens outside the uterus, usually in a fallopian tube. Talk with your doctor right away if you have a positive pregnancy test after the Essure procedure.
After you have the Essure system implanted, you may not be able to have pelvic procedures involving electrosurgery, such as some types of endometrial ablation.
The Essure system doesn’t offer protection from sexually transmitted infections (STIs).
Long-Term Use Considerations
Patients may go home immediately after the procedure and return to your normal activities the same day. The most common side effects after the procedure are:
- Cramping
- Abdominal pain
- Nausea or vomiting
Patients must use another form of contraception for three months after the procedure. Around this time, a health care provider will order X-rays or other imaging tests to confirm the coils are in the right position and the fallopian tubes are blocked. If the procedure is successful, patients can stop using other forms of birth control at this point.
The Essure system doesn’t affect the monthly menstrual cycle. The Essure system cannot be reversed.
When To Stop Taking
The Essure system isn’t right for everyone, however. Your health care provider may recommend other methods of contraception if:
- You aren’t sure whether or not you want to become pregnant in the future.
- You have a metal allergy. The materials used in the inserts may contain traces of nickel or other metals. You may need allergy testing before the procedure.
- You’re allergic to the contrast (dye) used during follow-up imaging tests to confirm the procedure worked.
- You have an autoimmune disease, which may trigger excessive inflammation around the coil inserts.
- You’ve had a baby or an abortion within the past six weeks.
- You have or recently had a pelvic infection.
- A health condition of the uterus or fallopian tubes blocks the tube openings, which means the doctor can’t properly place the Essure system.
- You’ve had your tubes tied (tubal ligation).
Long-Term Side Effects
Most women report no long-term side effects.
FDA Warnings (History Of)
The product was approved by the FDA in 2002. In 2013, the product made news in North America, with women complaining of severe side effects leading to surgical extraction. According to one article, women who have gotten pregnant are naming these children e-babies.
In October 2013 the FDA stated that since the product was approved in 2002 it had received 943 reports of adverse events related to Essure, mainly for pain (606 of the complaints). An additional 1,000 more complaints have been sent to the FDA in a voluntary reporting system, but physicians are not obliged to report complaints.
In June 2015, the FDA reported an investigation into Essure and its over 5000 complaints, seven reported deaths, and many additional side effects, all linked to Essure, its specific chemical composition, its improper placement and its insertion. The agency announced that its Obstetrics and Gynecology Devices Panel would conduct an evidence-based review of Essure’s safety in September 2015 due to the rise in adverse event reports from only 950 reports between 2002 through October 2013, to more than 4,150, or 81 percent of the total, from October 2013 to June 2015.
In February 2016, the FDA issued a “black box” label to warn the public about the harmful complications associated with the use of this device and requested Bayer to conduct a new postmarket surveillance to follow 2,000 women for at least three years, comparing the effectiveness and safety of the device with other surgical contraceptive methods. Women and doctors were required to sign a decision checklist before Essure implantation, and to give consent to a test three months later to ensure the device was properly placed and functioning.
In 2018, the FDA restricted the sale and use of Essure.
Lawsuits
While Bayer has been under fire for many of their products, they are currently facing more than 18,000 lawsuits over their implantation method of female sterilization, Essure. Women all over the United States are suing the pharmaceutical giant for serious side effects that occurred as a result of the defective device.
Conceptus Inc, the original manufacturer of Essure, was obtained by Bayer in April of 2013. Around the same time, a slew of adverse events was reported to the U.S. Food and Drug Administration (FDA) regarding the permanent birth control device. Women have reported the development of autoimmune disorders, migrating devices, and unintended pregnancies. There is even evidence that suggests that the manufacturer failed to report many adverse events they knew about and altered records to show favorable information.
In April 2018, the FDA restricted sale and use of Essure. On July 20, 2018 Bayer announced the halt of sales in the U.S. by the end of 2018.
https://www.mayoclinic.org/tests-procedures/essure/about/pac-20394017
