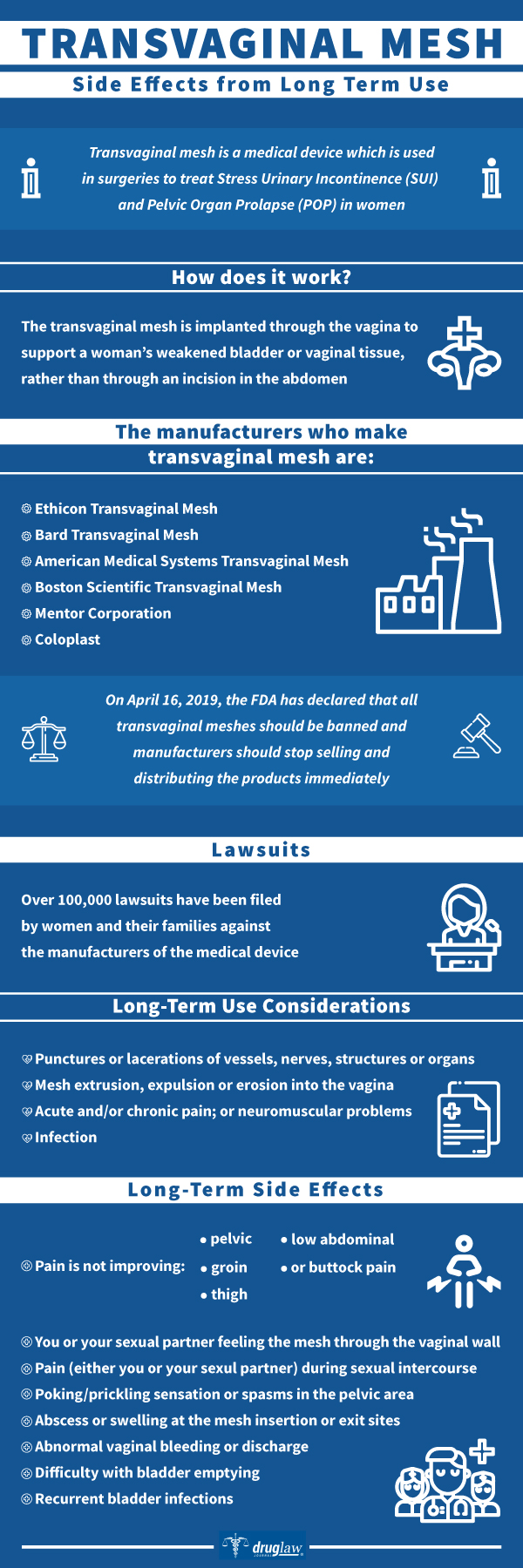
Transvaginal mesh is a medical device which is used in surgeries to treat Stress Urinary Incontinence (SUI) and Pelvic Organ Prolapse (POP) in women. The transvaginal mesh is implanted through the vagina to support a woman’s weakened bladder or vaginal tissue, rather than through an incision in the abdomen.
Prescription Name and Overview
A pelvic mesh/ transvaginal mesh/ urogynecologic surgical implant is a woven synthetic netting implanted in a surgical procedure through the vagina. It is implanted into the pelvis for reasons such as pelvic organ prolapse and stress urinary incontinence.
There are four types of surgical meshes: non-absorbable polyester or polypropylene, absorbable synthetics, animal tissues, and combinations of the above. Many of the urology surgeries are done using the polyester or polypropylene mesh.
Generic Name and Overview
A generic (unbranded) version of the transvaginal mesh is not available.
OTC Name and Overview
This medical device is not available for over-the-counter purchase.
Manufacturer
The manufacturers who manufacture transvaginal mesh are:
- Ethicon Transvaginal Mesh- a subsidiary of the health giant, Johnson & Johnson
- Bard Transvaginal Mesh
- American Medical Systems Transvaginal Mesh
- Boston Scientific Transvaginal Mesh
- Mentor Corporation
- Coloplast
Labeled Indications
Transvaginal mesh is used to treat:
- Pelvic organ prolapse (POP)- this happens when the muscles and ligaments on a woman’s organs on the pelvic area weaken and the organs slip out of their place (prolapse).
- Stress urinary incontinence (SUI)-this happens when there is unintentional release of urine due to a physical activity. These physical movements put stress on the bladder and cause the urine to leak, such as: coughing, sneezing, running, laughing, or lifting heavy objects.
Active Ingredients
NA
What Is It Used For?
Surgical mesh has been used for urogynecologic procedures, including repair of pelvic organ prolapse (POP) and stress urinary incontinence (SUI).
How Does it Work?
Surgical mesh is a medical device that is used to provide additional support when repairing weakened or damaged tissue.
The transvaginal mesh is permanently implanted to reinforce the weakened vaginal wall for POP repair or support the urethra or bladder neck for the repair of SUI.
What are the Approved Uses?
The FDA has approved three main surgical procedures performed with surgical mesh to treat pelvic floor disorders with surgical mesh:
- Transvaginal mesh to treat POP
- Transabdominal mesh to treat POP
- Mesh sling to treat SUI
Each of these procedures has unique risks and benefits and it is important not to confuse the procedures and their risks and benefits.
POP and SUI are different but both may occur to the same woman, and the surgeries for the two conditions may be performed together. In most cases:
- The recommended first line treatment for either condition is with a pelvic physiotherapist and urogynaecology nurse who are trained in pelvic floor problems, except in severe prolapse as outlined above.
- Women can safely choose to have no treatment and prefer to manage with pads or other treatment/aids.
- Treatment is usually only recommended if prolapse or incontinence symptoms are bothersome, or there is an extremely large prolapse creating bladder blockage, kidney blockage, vaginal ulceration or pelvic pain.
- Women should consider conservative (non-surgical) treatment before considering surgical treatment.
- Surgery for both prolapse and stress incontinence generally involve procedures that reinforce the weakened support tissues.
- Many women choose to go on to surgery because they have not gained sufficient improvement with non-surgical treatments, and the condition is affecting their quality of life.
Production Anecdotes / History
The majority of surgical mesh devices currently available for use are made from synthetic materials or animal tissue. The use of mesh for surgeries started in the 1950s. It was basically used for hernia repair.
In the 1970s, GYN surgeons started to use the mesh designed for hernia repair to help support the tissues in the vagina to repair pelvic organ prolapse (POP).
In the 1990s, surgeons began using mesh to treat stress incontinence (SI) in patients who experience loss of urine with coughing, sneezing, jumping, etc.
In 1996, FDA approved a mesh for specific use in SI surgeries. In 2002, the first mesh device specific for POP was approved and cleared for use by the FDA. In succeeding years, the transvaginal mesh had been widely used. However, years after “successful” surgeries, the FDA gathered thousands of reports of women experiencing complications or symptoms like persistent vaginal bleeding or discharge, pain in the pelvis or groin, pain in having sexual intercourse, and other symptoms.
On April 16, 2019, after a year-long investigation, the FDA has declared that all transvaginal meshes should be banned and manufacturers should stop selling and distributing the products immediately. They were given 10 days to submit a plan how to do this. “We couldn’t assure women that these devices were safe and effective long term.” Dr. Jeffrey Shuren, director of the FDA’s Center for Devices and Radiological Health said.
“Although we welcome this long-overdue action, this ban comes too late for the thousands of women who who have been irreparably harmed by these devices.”, Dr. Michael Carome, director of the Health Research Group under Public Citizen, a consumer advocacy organization.
Discontinued transvaginal mesh products are:
- ProtGen by Boston Scientific Corporation
- ObTape by Mentor Corporation
- Avaulta Plus by C.R.Bard Incorporated
- Gynecare Prolift by Ethicon (Johnson & Johnson)
- Gynecare Prolift + M by Ethicon (Johnson & Johnson)
- Gynecare Prosima Pelvic Floor Repair System by Ethicon (Johnson & Johnson)
- Apogee Vault Suspension System by American Medical Systems (AMS)/Endo Pharmaceuticals
- Apogee Pelvic Floor System by AMS/Endo Pharmaceuticals
- BioArc Sling System by AMS/Endo Pharmaceuticals
- In-Fast Ultra Transvaginal Sling, by AMS/Endo Pharmaceuticals
- Perigee System by AMS/Endo Pharmaceuticals
On March 2019, CR Bard has ended its production and marketing of its mesh business and on April 16, 2019, the two manufacturers, Boston Scientific and Coloplast were also ordered by the FDA to stop manufacture and withdraw their mesh products from the market.
Precautions
Many of the women who underwent transvaginal mesh procedures had a good outcome, however, there are an overwhelming number who have suffered complications. Some of these complications are serious and changed their lives, some experienced severe chronic pain, some had their meshes erode into the bladder, urethra, and bowel, while others had recurrent infection.
Long-Term Use Considerations
One of the biggest problems for women who have undergone the transvaginal mesh procedure is the long-term complications that arise after their surgery.
While at first, it seems that the problem has been addressed, some possible complications have surfaced after some time. Some complications include:
- Punctures or lacerations of vessels, nerves, structures or organs, including the bladder, urethra or bowel, requiring surgical repair.
- Mesh extrusion, expulsion or erosion into the vagina or other structures or organs.
- Acute and/or chronic pain; or neuromuscular problems.
- Infection.
Long-Term Side Effects
Some long-term side effects that may mean you have a mesh complication:
- Pain is not improving- low abdominal, pelvic, groin, thigh, or buttock pain
- poking/prickling sensation or spasms in the pelvic area
- You or your sexual partner feeling the mesh through the vaginal wall
- Pain (either you or your sexul partner) during sexual intercourse
- Abnormal vaginal bleeding or discharge
- Difficulty with bladder emptying
- Recurrent bladder infections
- Abscess or swelling at the mesh insertion or exit sites.
FDA Warnings (History Of)
Transvaginal meshes have been used in over a million surgeries, majority of these having serious complications right after. More than 100,000 lawsuits have been filed against transvaginal mesh manufacturers. Due to this fact, on April 16, 2019, the FDA has ordered that all remaining surgical mesh products indicated for the transvaginal repair of pelvic organ prolapse (POP) to stop selling and distributing their products in the US immediately. The order is the latest in a series of escalating safety actions related to protecting the health of the thousands of women each year who undergo surgery transvaginally to repair POP.
The FDA first issued a public health warning on October 20, 2008 that there were over a thousand cases of complications that happened with the transvaginal mesh procedure. These complications include bowel or bladder perforation, vaginal scarring, mesh erosion, pain during sex, infections, chronic pain.
In January 2011, the FDA issued another public warning that there were almost 3,000 cases of reported complications due to the mesh, including recurrence of POP and SUI. This time, the FDA also launched an investigation on all published scientific literatures from 1996-2011, and found out that the mesh surgery did not improve the quality of life nor the symptoms using transvaginal mesh over non-mesh repairs.
Other Common Side Effects
- Pain or discomfort of the vagina or in the surrounding pelvic region
- Nerve damage including pain or loss of sensation in the vagina or surrounding pelvic region
- Scarring of the vaginal walls
- Shrinkage of the vagina
- Pain during intercourse
- Recurrence of POP or SUI
- New occurrence of SUI
- Recurring urinary tract infection
- Increased risk of Infection
- Excessive vaginal bleeding
- Erosion of the vaginal wall
- Vaginal or other organ perforation
- Need for revision surgery
- Emotional trauma
Some serious side effects are:
- Transvaginal Mesh Erosion
- Transvaginal Mesh Organ Perforation
- Transvaginal Mesh Revision Surgery
Lawsuits
Over 100,000 lawsuits have been filed by women and their families against the manufacturers of the medical device. These manufacturers are:
- Ethicon (Johnson & Johnson)
- American Medical Systems (Endo International)
- CR Bard, including TSL and Sofradim products
- Coloplast Corp
- Boston Scientific
- Cook Medical Inc
- Neomedic International
- Medtronic (including Coviden and Tyco products)
- Caldera Medical
More than 10,000 lawsuits have been settled so far, and the manufacturers have already paid more than $1.2 Billion for the claims. But there are still more than 60,000 cases pending in the courts. Some examples of these settlements are:
- A California couple was given $5M settlement with Bard in 2012
- A TX woman was given $34.6 M settlement in 2014 against Ethicon/ J&J.
- In 2015, 3,000 Boston cases were settled for $119 M.
If you have been injured or has experienced complications or have been required to go through revision surgery after being treated with a transvaginal mesh procedure, you may be eligible for compensation. These medical settlements compensate for your medical costs, lost wages, permanent injury or permanent disability, loss of spousal relationship, medical costs that may come because of your complications, pain and suffering, untimely death.
https://www.drugdangers.com/transvaginal-mesh/revision-surgery/
https://blogs.webmd.com/womens-health/20110801/vaginal-mesh-new-fda-warnings

